By Doyle Rice, USA TODAY
One hundred years ago, death came with astonishing speed and horrifying agony.
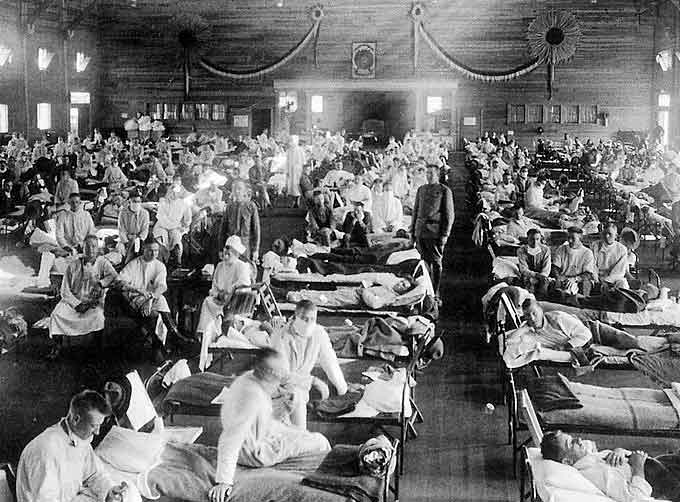
Some influenza patients admitted to a Boston hospital in the morning of October 1918 would be dead by the evening, their bodies turning blue from lack of oxygen.
Hospitals reported an average 100 deaths a day, overwhelming morgues.
(Learn More. The 1918 Flu Pandemic – Science and History Documentary. Courtesy of Tony Garcia and YouTube. Posted on Jan 10, 2017.)
Up to 500 million people – about one-third of the world’s population – became infected with the influenza virus, the Centers for Disease Control and Prevention says.
As many as 50 million died, or one out of every 30 human beings on the planet, killing more American troops than those that died on World War I battlefields.

The intensity and speed with which it struck were almost unimaginable, the worst global pandemic in modern history.
Most chilling is that such a calamity could again occur today.
“A global influenza pandemic is No. 1, 2, 3 and 4 on our list of the most-feared public health crises,” according to Michael Osterholm, director of the University of Minnesota’s Center for Infectious Disease Research and Policy.
Another expert, Vanderbilt University infectious disease specialist William Schaffner, said “we fear flu. We know how serious it is.”
(Bill Gates thinks there’s a new flu epidemic lurking just around the corner and he says we’re unprepared for it. The billionaire philanthropist warned that there is a “significant probability of a large and lethal modern-day pandemic occurring in our lifetimes.” Courtesy of Wochit News and YouTube. Posted on Apr 27, 2018.)
It could happen again
Top health and science groups, such as the World Health Organization, the National Academy of Sciences and the Centers for Disease Control and Prevention, predict influenza pandemics are nearly certain to recur.
“Influenza viruses, with the vast silent reservoir in aquatic birds, are impossible to eradicate,” the World Health Organization warned.
“With the growth of global travel, a pandemic can spread rapidly globally with little time to prepare a public health response.”
A pandemic could also arise if a strain mutates with or develops directly from animal flu viruses, the CDC said.
The main contributors to a potential pandemic are the lack of a universal vaccine and humans’ lack of immunity to those potential unborn strains.
(Learn More. 100 years ago the 1918 influenza pandemic devastated entire communities and took at least 675,000 American lives. It was the most severe pandemic in recent history, sweeping the globe quickly and killing more than 50 million people. This video provides information and background on the 1918 flu pandemic. Courtesy of the Centers for Disease Control and Prevention (CDC) and YouTube. Posted on Jun 5, 2018.)
“The threat of a future flu pandemic remains,” the CDC said. “A pandemic flu virus could emerge anywhere and spread globally.”
If an equal ratio of Americans died in a pandemic today, that would be an unimaginable 2 million Americans. That’s the current population of the entire Las Vegas metropolitan area.
In a near worst-case scenario, a new, lethal and highly infectious flu virus would break out in a crowded, unprepared megacity that lacks public health infrastructure, according to Johns Hopkins’ Bloomberg School of Public Heath.
Such a fast-moving virus could burst from a city and catch a ride with international travelers before public health officials realize what is happening.
Specifically, avian influenza viruses such as H7N9 top pandemic threat lists, according to Johns Hopkins.
While these strains are mostly harmless in chickens, they could potentially evolve into much deadlier strains for humans.
“In terms of pandemic potential, an avian influenza virus is thought to be a likely candidate, based on prior pandemics,” says Amesh Adalja of the Center for Health Security at the Johns Hopkins Bloomberg School of Public Health.
However, there are safeguards to detect and counteract influenza outbreaks that did not exist 100 years ago.
These include systems to detect signs of potential outbreaks around the world, Schaffner said.
In addition, he said scientists have the capacity to make vaccines more rapidly and also have better antiviral drugs that could be used to treat those who contract the disease.
Still, influenza and the potential for a pandemic are concerns that are always at the top of the list for experts who work with infectious diseases and public health, he said.
Pandemics ignore national borders, social class, economic status, and even age.
(It’s the time of year to get your flu shot. The CDC said everyone 6 months and older should get the shot. Courtesy of ABC Action News and YouTube. Posted on Sep 17, 2018.)
1918 pandemic
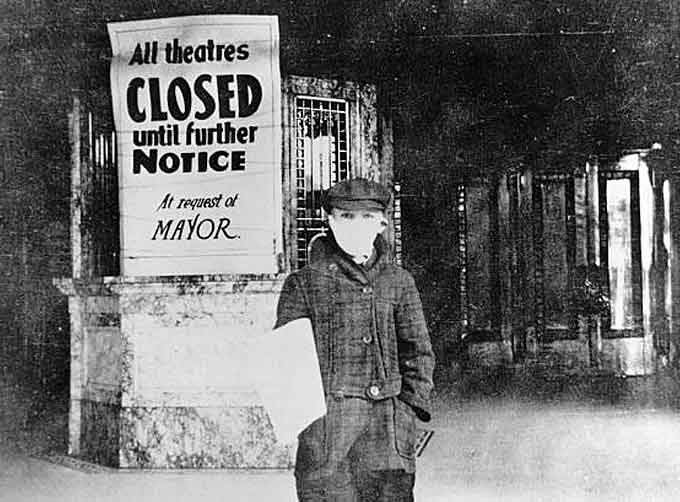
Spreading from birds to humans, the 1918 pandemic might have started in Kansas. Or France, or maybe Asia, according to Olsterholm.
What is known is that it was caused by an H1N1 virus with genes of bird origin.The First World War, about to come to its horrific end in Europe in November 1918, may have played some role in moving the virus around the world. “But we can’t say that the war was the cause,” he said.
It was “a widespread, worldwide pandemic.
It was a virus no one had ever seen before,” said Dr. Paul Offit, director of the vaccine education center at the Children’s Hospital of Philadelphia.
The pandemic killed more people in 24 months than AIDS killed in 24 years, more in a year than the Black Death killed in a century, according to the book “The Great Influenza.”
The dead included about 675,000 people in the United States. In just October alone, the worst single month in the U.S., an unthinkable 100,000 Americans died.
Many were young adults in the prime of their life.
“The high mortality in healthy people, including those in the 20- to 40-year age group, was a unique feature of this pandemic,” the Centers for Disease Control said.
The World Health Organization said the 1918 influenza pandemic was known colloquially as “Spanish flu,” although there was nothing “Spanish” about the epidemic.
Flu today and how to protect against it
Although every flu season is different, and influenza infection can affect people differently, millions of people get the flu every year, according to the CDC.
Hundreds of thousands of people are hospitalized and thousands or tens of thousands of people die from flu-related causes every year.
An annual seasonal flu vaccine is the best way to help protect against flu, the CDC said. Everyone 6 months of age and older should get a flu vaccine every season.

Even if it’s only 40 percent effective, that’s still better odds than doing nothing at all, Offit said. “Influenza knocks you out.”
Vaccination has been shown to have many benefits, including reducing the risk of flu illnesses, hospitalizations and even the risk of flu-related death in children.
Osterholm recommends getting the shot as close to the heart of flu season as possible, since the duration of protection is limited.
As what a citizen can do to prevent a future pandemic, though a seasonal vaccine would be ineffective, he said the best action is to reach out to the government and tell them to start working on new vaccines for influenza.
“There are potentially new pandemic strains out there,” he said. “But we’ve invested very little in influenza vaccines.”
Learn More…
By the Centers for Disease Control and Prevention
Vaccination Remains Your Best Flu Protection
 The best way to prevent flu and its potentially serious complications is getting a flu vaccine.
The best way to prevent flu and its potentially serious complications is getting a flu vaccine.
Fall brings cooler temperatures, colorful leaves, and football games.
It also means another flu season is upon us. Last year’s was rough.
The CDC classified 2017-2018 a high severity season with high levels of outpatient clinic and emergency department visits for influenza-like illness, high influenza-related hospitalization rates, and widespread influenza activity across the United States for an extended period.
The CDC estimates the flu caused between 140,000 and 710,000 hospitalizations and between 12,000 and 56,000 deaths annually in the U.S. since 2010.
While estimates for last season won’t be available until later in the fall, it’s likely that last season was record-breaking across both of these key indicators used to track severity.
It’s not possible to predict how severe the upcoming season will be, but we know that the best way to prevent flu and its potentially serious complications is a flu vaccine.
Flu viruses infect the nose, throat, and lungs and can cause a wide range of complications. Sinus and ear infections are examples of moderate complications from flu.
Pneumonia is a serious flu complication that can result from either flu virus infection alone or from co-infection of flu virus and bacteria.
Flu virus infection can also cause serious complications like inflammation of the heart (myocarditis), brain (encephalitis) or muscle (myositis, rhabdomyolysis), and multi-organ failure (for example, respiratory and kidney failure).
Flu can also trigger an extreme inflammatory response in the body and can lead to sepsis, the body’s life-threatening response to infection.
The U.S. experienced high rates of hospitalization and severe disease during the past seven flu seasons.
(Learn More about important influenza (flu) prevention actions, including receiving a flu vaccine every year. Preventive actions, including covering your nose and mouth when you sneeze or cough and limiting your contact with others if you become sick, can also help prevent the spread of flu. Courtesy of the Centers for Disease Control and Prevention (CDC) and YouTube. Posted on Apr 5, 2017.)
Flu vaccination can help keep you from getting sick from flu.
Protecting yourself from flu also helps protect the people around you who are more vulnerable to serious flu illness.
People at High Risk of Flu Complications:
- Children younger than 5, but especially younger than 2 years old;
- People 65 and older;
- People with asthma, heart disease, chronic lung disease, and neurological and neurodevelopmental conditions;
- People with blood, kidney, liver, endocrine, and metabolic disorders, including diabetes mellitus;
- People who have a weakened immune system due to disease or medication;
- Pregnant women and women up to two weeks postpartum;
- Residents of nursing homes and other long-term care facilities.
For the full list of high-risk conditions, visit People at High Risk of Developing Flu-Related Complications.
CDC recommends a yearly flu vaccine for everyone 6 months of age and older as the first and most important step in protecting against this serious disease.
While the flu vaccine can vary in how well it works, it is the best tool modern medicine currently has to prevent infection with influenza viruses.
CDC estimates that for the 2016-2017 flu season, nearly 47 percent of the population were vaccinated.
Influenza vaccination prevented an estimated 5.3 million illnesses, 2.6 million influenza-associated medical visits, and 85,000 hospitalizations associated with influenza.
CDC experts calculated that a 5 percentage point increase in vaccination rates could have prevented another 483,000 influenza illnesses, 232,000 influenza-associated medical visits, and 7,000 influenza-associated hospitalizations across the U.S. population.
We know that flu illness can be serious and that flu vaccine can prevent illness.
Let’s clear up some issues that discourage people from getting vaccinated:
- A flu vaccine cannot give you flu.
- The most common side effects from a flu shot are soreness, redness and/or swelling where the shot was given, fever, and/or muscle aches.
- These side effects are NOT flu.
- If you do experience side effects, they are usually mild and short-lived, especially when compared to symptoms from a bad case of flu.
- Flu vaccines are among the safest medical products in use.
- Hundreds of millions of Americans have safely received flu vaccines over the past 50 years.
- Extensive research supports the safety of flu vaccines.
- CDC and the Food and Drug Administration (FDA) closely monitor the safety of vaccines approved for use in the U.S.
Reasons to Get a Flu Shot
- Flu vaccine has been shown to reduce flu illnesses and reduce the risk of flu hospitalization, ICU admission and even death in children.
- Flu vaccination also is an important preventive tool for people with chronic health conditions. (heart disease, lung disease, diabetes)
- In addition to helping to protect pregnant woman from flu illness and hospitalization, a flu vaccine given during pregnancy has been shown to help protect the baby from flu infection for several months after birth, before he or she is old enough to be vaccinated.
- A 2017 study showed that flu vaccine can be life-saving in children.
- Flu vaccination also may make your illness milder if you do get sick.
- (For example a 2017 study showed that flu vaccination reduced deaths, intensive care unit (ICU) admissions, ICU length of stay, and overall duration of hospitalization among hospitalized flu patients.)
What flu vaccines are available this season?
For the 2018-2019 flu season, options include:
- Standard dose flu shots. These are given into the muscle.
- They are usually injected with a needle, but two (Alfluria and Alfluria Quadrivalent) can be given to some people (those aged 18 through 64 years) with a jet injector.
- High-dose shots for older people. Flu vaccines are among the safest medical products in use.
- Hundreds of millions of Americans have safely received flu vaccines over the past 50 years. Extensive research supports the safety of flu vaccines.
- CDC and the Food and Drug Administration (FDA) closely monitor the safety of vaccines approved for use in the U.S.
- Shots made with adjuvant for older people.
- Shots made with virus grown in cell culture.
- Shots made using a vaccine production technology (recombinant vaccine) that does not require the use of flu virus.
- Live attenuated influenza vaccine (LAIV) – or the nasal spray vaccine – is approved for use in non-pregnant individuals, 2 years through 49 years of age. There is a precaution against the use of nasal spray flu vaccine in people with underlying medical conditions.
CDC and its vaccines advisory committee (ACIP) recommend providers use any licensed, age-appropriate flu vaccine with no preference for one vaccine over another.
It’s best to get vaccinated before flu begins spreading in your community. It takes about two weeks after vaccination for your body to develop protection against flu.
This flu season protect yourself, your family, your friends, and your community. Get a flu vaccine by the end of October.
Talk to your health care provider if you have questions about the benefits of flu vaccination. Flu vaccine provides protective properties even in years the vaccine does not closely match the flu viruses in circulation.
For more information about vaccine effectiveness, visit How Well Does the Seasonal Flu Vaccine Work?
Along with CDC, the American Academy of Pediatrics, the American Medical Association, the National Foundation of Infectious Diseases, and many other professional medical groups recommend an annual flu vaccine.
Many people choose not to get vaccinated thinking that they do not work, or that the flu vaccine will give them the flu. Years of research disproves those misconceptions.
 Don’t skip getting a flu vaccine!
Don’t skip getting a flu vaccine!
Where to Get Vaccinated:
Flu vaccines are offered in many locations, including doctor’s offices, clinics, health departments, pharmacies and college health centers, as well as by many employers, and even in some schools.
To find flu vaccine in your area use the HealthMap Vaccine Finder.
Original post https://blogs.cdc.gov/publichealthmatters/2018/05/1918-flu/