Guest Editorial by Jeff Weinstein, a paramedic and a Medical Operations Supervisor for Global Rescue
Wet year. Mild winter. Early spring. This combo creates ideal conditions for an engorged tick season in 2021. Experts predict a record year with tick populations skyrocketing across many parts of the U.S.
That translates to higher possibilities of tick-borne diseases.
But, because they are so small — sometimes the size of a sesame seed — ticks can be difficult to spot before they’ve attached to you or another host in your household, like a child or dog/pet.
While there are 90 different species of ticks in the U.S., only eight are the ones that can make you sick.
The Northeast’s Deer Tick may be most notoriously known as it can transmit two types of bacteria that result in Lyme disease, but there is also the Lone Star Tick (responsible for Alpha-Gal Syndrome, a sudden allergy to red meat); the Brown Dog Tick, American Dog Tick, and Gulf Coast Tick (all carriers of Rocky Mountain Spotted Fever); The Rocky Mountain Tick (Colorado Tick Fever); the Western Blacklegged Tick (Anaplasmosis, Babesiosis and Lyme disease); and finally, the Soft Tick (Tick-Borne Relapsing Fever).

Tick-associated illnesses sound scary and can be dangerous, but if you receive a fresh bite, don’t panic: A tick bite doesn’t mean you’re guaranteed to be infected with a disease.
Ticks are not born with bacteria or viruses. They are vectors and transmit diseases by feeding on one infected host and then passing along those pathogens to the next.
No pathogens? No problem.
But you won’t know in advance so it’s necessary to take precautions, especially in a high tick season, to protect yourself before heading out into tick-heavy territory, and after you return.
Here are 8 pro tips to consider.
Walk in the center of trails and avoid high grass.
-
Ticks live in grassy and wooded areas where they wait with their legs outstretched to the sky in a position known as “questing” until someone brushes up against them when they grab ahold and settle in.
Reduce exposed skin and tie up loose hair.
-
Ticks seek out warm spots on your skin to embed. Wearing enclosed shoes, long-sleeved shirts, and tucking your pants into your socks helps deter tick advances. Keep your hair tied back or tucked into a hat to avoid giving them any easy platforms to grip on to.
Wear light color clothing.
-
It makes ticks easier to spot if they hitched aboard.

Treat your clothing or consider using repellents.
-
If you’re going to be outside in wooded, grassy areas or in the backcountry, it’s a good idea to apply insecticide permethrin to your gear and clothing. Applications last for several washes. You can use EPA-approved repellant sprays on uncovered skin.
If you find an embedded tick, do not panic.
-
First, ignore the folklore remedies, such as “painting” the tick with nail polish or petroleum jelly to suffocate it or using the “hot-match” technique to make it back out. These methods can cause the tick to burrow deeper and discharge more potentially infectious secretions. Here’s how to remove a tick safely.
Get the proper tools.
-
While a pair of clean fine-tipped tweezers work just fine, there are plenty of different types of tick-removal tools on the market, including tick keys, tick “scoops” and “twisters.” Never use your fingers and have rubbing alcohol handy for cleaning the bite site after removal.
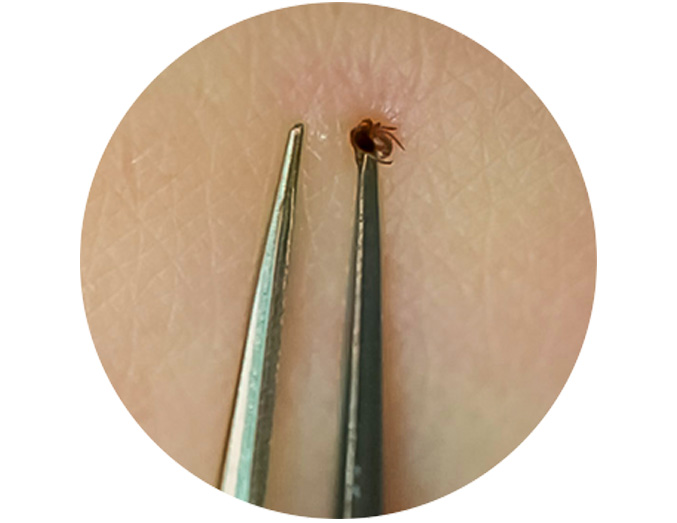
Pull steadily and securely.
-
Grasp the tick as close to the skin’s surface as you can — near the head or mouth. Do not pull or squeeze the tick body since it can cause it to spill its stomach contents into the bite wound. Pull using even pressure. Never wiggle or twist as this can cause the head or mouthpart to break off and remain in the skin. If that does happen, use the tweezers to remove.
Dispose of the tick and clean up.
-
Flush the tick, or place it in rubbing alcohol to kill it. You can also seal the tick in a bag to dispose of later (but keeping the tick for identification by a healthcare provider can prove helpful should you fall ill). Thoroughly clean the bite area, your hands, as well as your tweezers with alcohol or soap and water.
It’s natural for a tick bite area to show some signs of immediate swelling or pain.
Pay attention to the development of symptoms in the coming days.
If headache, fever, stiff neck, muscle or joint pain or a rash (like the bull’s-eye rash commonly seen from Lyme) occur, that’s when you’ll want to see your doctor. Early detection and treatment greatly reduces the risk of serious complications.
About the Author

Jeff Weinstein is a paramedic and a Medical Operations Supervisor for Global Rescue, a world leading provider of medical, security, evacuation and travel risk management services to enterprises, governments and individuals.
Global Rescue has been a leader and pioneer in the travel services industry since our founding in 2004, providing integrated medical, security, travel risk and crisis management services available anywhere, delivered by their teams of critical care paramedics, physicians, nurses and military special operations veterans.
The company’s medical advisory and evacuation services include exclusive relationships with the Johns Hopkins Department of Emergency Medicine Division of Special Operations, Elite Medical Group and Partners HealthCare.
Global Rescue’s track record has made them a chosen provider to government agencies and some of the world’s largest companies, universities, nonprofits and tour operators.
Their mission is simple – to be there when it matters most.
(Learn More about Global Rescue for medical evacuation, security extraction, crisis response. Courtesy of Global Rescue and YouTube.)
Learn More…
To Learn More about Tick Bite Prevention, go to cdc.gov/ticks/tickbornediseases/tick-bites-prevention.html.
For further information on tick-borne diseases, please visit the Centers for Disease Control and Prevention (CDC) website at cdc.gov/ticks/tickbornediseases/index.html.
(Learn More about Rocky Mountain Spotted Fever in this training video which discusses the clinical signs and symptoms, diagnosis, and treatment of this disease, to provide information to help frontline healthcare providers recognize and treat this rapidly progressive, fatal disease. RMSF is the most severe rickettsiosis in the United States, with mortality rates as high as 25 percent in untreated cases. Courtesy of the Centers for Disease Control and Prevention (CDC) and YouTube.)
AST strives to meet a 3 STAR trustworthiness rating, based on the following criteria:
- Provides named sources
- Reported by more than one notable outlet
- Includes supporting video, direct statements, or photos